 I need to apologize for my lack of frequent blogging over the past month. Since my father’s passing, I have been struggling about my focus here. I absolutely want to continue to provide caregivers with education and encouragement so that I can empower them to be better caregivers. And I do realize that there are all kinds of caregivers: those who live with their care recipient, those who are long-distance caregivers, those who manage their aging parent or loved one’s finances, those who coordinate care of their parent in their parent’s home and those who oversee that their parent or loved one is well cared for in a facility or retirement community.
I need to apologize for my lack of frequent blogging over the past month. Since my father’s passing, I have been struggling about my focus here. I absolutely want to continue to provide caregivers with education and encouragement so that I can empower them to be better caregivers. And I do realize that there are all kinds of caregivers: those who live with their care recipient, those who are long-distance caregivers, those who manage their aging parent or loved one’s finances, those who coordinate care of their parent in their parent’s home and those who oversee that their parent or loved one is well cared for in a facility or retirement community.
My conflict comes from the conditions under which my father passed.
Consider this scenario for a moment. Imagine a man being admitted to a hospital who already has some comprehension that he is not going to live much longer and that being admitted is yet another BAD sign. Then imagine that nurses and physicians perform tests and procedures without consideration of the amount of pain that he is suffering. Add to this the fact that every day for the past 78 years, this man has had 3-4 cups of coffee and usually enjoys a nice glass of wine at night but that with the hospital admission, all of that is taken away. Imagine now that this man has dementia and does not recognize where he is or who these strange people are that keep entering and exiting his room.
Is there any wonder why he would become agitated? I, myself, become agitated if I don’t get my morning coffee and that’s just one part of the picture.
2 days after my father was admitted to the hospital, he lost his ability to know who I was. On day 3, he lost his ability to communicate effectively at all. When my father was transferred from the hospital to the skilled nursing facility, his arms were covered with bandages – still oozing blood on them “from trying to hit the nurses” I was told. This is a man who is ALWAYS cheerful and happy just to BE.
My father died 4 days after being admitted to the skilled nursing facility. Each day when I arrived to see him, he was restrained into a wheelchair and propped at the nursing station (along with many other restrained wheelchair bound patients). I was horrified ! To say I was unhappy with his treatment in BOTH places would be like saying “I kinda don’t like war”. I know in my heart that my father said “this is crap!” and decided to check out!
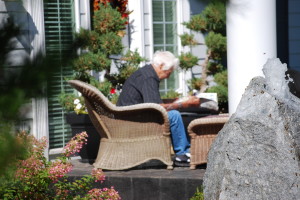
The reason I am writing about this is not to complain, but to say that this scenario could have been different. My father’s doctor could have told me things they neglected to tell me. Doctors need to stop beating around the bush saying “well, he might live another year” and help families set things in motion so that elders can qualify for hospice care and can die at home, in peaceful surroundings, being able to drink their coffee, sip a bit of wine, sit on the patio if their energy allows or lie in their own beds for as long as they want and not be lined up in wheelchairs like a bunch of zombies!
If I am passionate about anything, I am passionate about this!! End-of- life care has to change ! Monies from Medicare and Medicaid need to be re-directed to help pay for care that is respectful of the life of the individual -that means more money for home care, more money for hospice, more money for equipment to keep elders safe in the first place.
So as I continue to support caregivers of all kinds and provide the best information that I can find to help make your job easier, I am also going to encourage you to have frank discussions with your care recipient’s physicians about future care choices and to please consider home care as one of the options……….because hospitals are not good places for our elders.
LEARN TO LOVE YOUR LIFE AGAIN
 Do you feel like you need to hit the REFRESH button on your life? Download our free guide and begin to create your best life yet!
Do you feel like you need to hit the REFRESH button on your life? Download our free guide and begin to create your best life yet!



AMEN to that. Hospitals are horrible places for the elderly. My mother entered one last April (walked in of her own accord) and after 3 weeks, left on a stretcher, unable to walk, feed herself or speak coherently. She was turned into an invalid for the convenience of the staff. This was due to her being a difficult dementia patient. Ironically, the nursing home she was transferred to found a med that helped her regain herself, they gave her PT, and she is now a functioning, walking person again. She was even able to leave the dementia unit and move to the regular part of the nursing home. But we have got to change the way our elderly are treated by medical professionals in hospitals. There is no respect, no dignity and no understanding of what it means to have quality of life at an advanced age.
You’re absolutely right ! A week before my father was admitted, we were playing Cribbage ! Nurses are just too busy ( this, I know from my own work experience) and their aids are too undereducated….and sometimes, they just don’t care.
Oh, Shelley … no wonder you’ve been so upset about your Dad’s last days.
I well remember going into the hospital and finding my Dad in restraints. I am angry again just thinking of it.
Later, as it became clear he wasn’t going to survive, we asked that he be moved to Hospice.
Hospice was still within the hospital, but it felt like another planet. (A wonderful planet.) Their whole orientation was about keeping Dad as comfortable as possible … AND they also focused on supporting us, the people who loved him.
I am now a passionate evangelist for Hospice — whether at home or in a hospital.
Oh Shelly, I couldn’t agree more! I, too, am very passionate about this topic. I am on the same side–but with a different view. I am a hospital doctor who sees this everyday and sometimes want to scream!
I have very little voice when I try to change the system one patient at a time, so I have written a book to try to help patients and families through a hospital stay. In it I explain that:
“there can be obstacles to dying in the hospital. The reality is that hospitals have long been places where sick people receive diagnostic tests and treatment in order to help them recover. The shift to “relief of symptoms only” can be difficult for the doctors, nurses, and other staff if they have not been trained to deal with dying patients.”
http://www.thehospitalbook.com
And I have a different opinion of Hospice. My husband was disagnosed “terminal” because of melignant melanoma two months before he died in 2001. The Hospice personnel in Grant County rarely visited and when they did, they were cold and couldn’t wait to leave.
The Home Health Care Aide who came twice a day to change his sheets and clean my husband up was the only person who helped me keep my sanity.
I was informed by Hospice that no matter the time when my husband died, they would be there to help. All I needed to do was make a phone call. I did at 2 AM on December 26th. The nurse who answered said “she couldn’t make it.” Her tone of voice told me she didn’t like being woke up.
So for 3 hours I sat next to my dead husband waiting for the creamation society to come from Spokane to pick up his body.
Alone and scared, I phoned the Deputy Coroner to make sure I would not be in trouble because there was nobody to pronounce him officially dead. She talked to me for 45 minutes and assured me it was fine. She even volunteered to come over.
There was more caring from her than I received from any of the personnel in Hospice.
So I will definitely not be campaigning for Hospice to receive any money. At least not in Grant County.
Do I agree that Hospitals do not leave a person with any dignity when a patient is dying? Yes! That’s why I agreed to my husband’s wishes that he die at home.
Would I do it differently now knowing what I know about Hospice? Yes, I would have left them out of the equation.
Judith
What a horrible experience for you, Judith !! I am so sorry. It’s unforgivable that you would be left alone like that.
Clearly there are many changes that need to be made within our health care system and a big change needs to be how to care for our aging and dying population. Reading Dr. Rokavec’s comment explains a lot about the hospital philosophy.
When I was referring to “hospice”, my idea was more that palliative cares would be done at home (and that a home health aide to spend the entire night aside the patient would be a covered expense, so that the primary caregiver could sleep and NOT be left alone).
Hi Shelly: What a terrible story. And a tough nut to crack esp. in this time of corporate hospitals where bottom line is everything – cost control rules. Doctors, nurses, patients – not even close. Susan Lyons has just begun to guest blog for us about the husband she is now caring for who is diagnosed w/ dementia. She is a journalist and loves him very much. But as you can imagine, it is difficult. Could you reach out to her w/ a comment? Her first entry is titled “A journal begins: “A Parallel Universe: Living Alongside Dementia”‘ http://tinyurl.com/6rkl5an
Jackie
Hi Jackie,
Thanks for your comment and I’d be delighted to respond to Susan’s post. I’ll do that NOW! 🙂